Introduction
The 2014 NHLBI Sickle Cell Expert Panel recommends that young adults with sickle cell disease (SCD) be supported to develop a reproductive life plan, but little data about implementing this recommendation exists and reproductive health behaviors or knowledge is not assessed in existing SCD transition readiness forms. Young adults with SCD confront typical age-related reproductive challenges and require additional support due to SCD-related complexities. For men and women, there are questions about the effect of SCD and its treatments on fertility and reproductive lifespan and the problem of genetic risk for SCD in offspring. For men, priapism and erectile dysfunction may be problems, while women face contraception choices and complicated pregnancy care. In our young adult clinic, we assess young adults' reproductive history, intentions and knowledge using a clinical survey and standard intake questions. The purpose of this study was to describe young adult responses to our family planning survey.
Methods
This is a retrospective analysis of patients who established care at the Johns Hopkins Sickle Cell Center for Adults' Young Adult Clinic (YAC), which serves young adults with SCD <31 years. The survey is administered to all new patients, consists of 10 questions and has a Flesch-Kincaid Grade Level score of 6. A systematic chart review captured respondent demographic data to characterize the responses.
Results
Fifty patients who established care in the YAC over its first 15 months (April 2019-July 2020) completed the survey. They were 66% female with a median age of 23.5 (IQR 21,25). Most (74%) had sickle cell anemia (SCA); 60% had education beyond high school. Most (78%) were either students (34%) or employed full time (44%). Forty-two percent lived with a parent. Most (68%) were sexually active, and 45% reported contraception use. Condoms were commonly used by both sexes (41%); forty percent of women used depot-medroxyprogesterone acetate (DMPA). Half of women (58%) had a gynecologist. One third of women reported dysmenorrhea. Forty-one percent of men reported priapism. Twenty-four percent of respondents had a history of pregnancy or of impregnating a partner and 14% had children. The median age of parents at the birth of the first child was 21 (IQR 16,22).
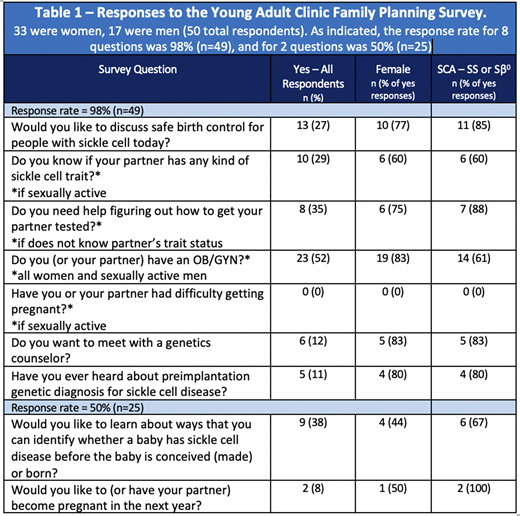
Survey results are in Table 1. The response rate was 98% for eight questions and 50% for two questions. Few (8%) reported desire to have a child in the next year, and 27% wished to discuss contraception. Among sexually active respondents, 29% knew their partner's sickle cell trait status and 35% of them wanted testing. Few respondents wanted to meet with a genetics counselor (12%) or reported knowledge of preimplantation genetic testing (PGT) (11%). Thirty-eight percent of respondents were interested in learning how to identify if a fetus has SCD.
Ninety-two percent of respondents indicated they do not desire pregnancy in the next year, and 38% of them were using contraception - 33% used condoms, 22% used DMPA, and 11% had an intrauterine device (IUD). Those interested in contraception were young (68% under 26), female (77%), and, of those women, most did not have a gynecologist (60%). Most women with dysmenorrhea (63%) were not interested in discussing contraception. Of the 14% of respondents with children, 29% knew their partner's trait status; and of those who did not, 20% wanted testing. Among 10 patients interested in genetic counseling or who knew of PGT, half had more than high school education; most (70%) were women with SCA who had never been pregnant. Among 82% who had not heard of PGT, 17% identified interest in more information. Most (70%) of this group was 22-25 years old, 14% wanted a child in the next year, all were either students (43%) or employed full time (57%); most (57%) had education beyond high school.
Conclusions
Clinic administration of a family planning survey is feasible. Many young adults transition to adult care and are parents or interested in becoming parents. Ninety-two percent of respondents do not desire pregnancy in the near future but 67% of them are not using reliable birth control. Genetic counseling interest, knowledge of PGT, and knowledge of partner sickle trait status is low. Current transition readiness documents for SCD do not adequately address reproductive health. These results suggest a discordance between the reproductive health priorities of young adults with SCD and providers that should be further examined.
Stewart:HRSA: Research Funding. Lanzkron:GBT: Research Funding; HRSA: Research Funding; Ironwood: Research Funding; NHLBI: Research Funding; PCORI: Research Funding; Pfizer: Research Funding; Pharmacy Times Continuing Education: Honoraria; Prolong: Research Funding. Pecker:Forma Therapeutics: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal